prevention of cervical
What is prevention?
- NChanging lifestyle or eating habits.
- NAvoiding things known to cause cancer.
- NTaking medicines to treat
A precancerous condition or to keep cancer from starting.
Different ways to prevent cancer are being studied, including:

KEY POINTS
- NReduced pain
- NAvoiding risk factors and increasing protective factors may help prevent cancer.
The following are risk factors for cervical cancer:
- NHPV infection
- NDES
In women who are infected with HPV, other risk factors add to the increased risk of cervical cancer:
- NGiving birth to many children
- NUsing oral contraceptives for a long time
- NSmoking cigarettes
The following increase the risk of HPV infection:
- NHaving a weakened immune system
- NBeing sexually active at a young age or having many sexual partners
The following protective factors decrease the risk of cervical cancer:
- NAvoiding sexual activity
- N Getting an HPV vaccine
- NUsing barrier protection during sexual activity
- NCancer prevention clinical trials are used to study ways to prevent cancer.
- NNew ways to prevent cervical cancer are being studied in clinical trials.
Avoiding risk factors and increasing protective factors may help prevent cancer.
Avoiding cancer risk factors may help prevent certain cancers. Risk factors include smoking, being overweight, and not getting enough exercise. Increasing protective factors such as quitting smoking and exercising may also help prevent some cancers. Talk to your doctor or other health care professional about how you might lower your risk of cancer.The following are risk factors for cervical cancer:
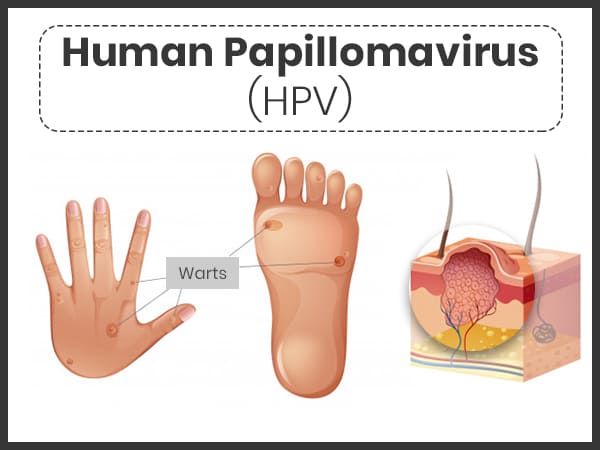
HPV infection
Cervical cancer is almost always caused by human papillomavirus (HPV) infection that is spread through sexual contact. There are more than 80 types of human papillomavirus and about 30 of these can infect the cervix. HPV types 16 and 18 are most often linked to cervical cancer.
Most of the time, the body’s immune system can fight the HPV infection before cancer forms. Only a very small number of women infected with HPV develop cervical cancer.
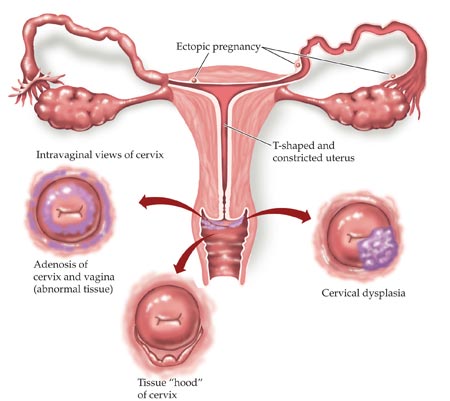
DES
Being exposed to a drug called diethylstilbestrol (DES) while in the mother’s womb increases the risk of cervical dysplasia and clear cell adenocarcinoma of the vagina and cervix. Between 1940 and 1971, DES was given to some pregnant women in the United States to prevent miscarriage (premature birth of a fetus that cannot survive) and premature labor.
In women who are infected with HPV, other risk factors add to the increased risk of cervical cancer:
Giving birth to many children
Among women who are infected with HPV, those who have had 7 or more full-term pregnancies have an increased risk of cervical cancer.